GUIDELINES FOR CHEMOTHERAPY CENTER DESIGN
Are you planning to build or restructure a Chemotherapy or Oncology center in India? Looking for detailed information about the design of Chemotherapy or Oncology center? In this article, Hospaccx Healthcare Consultancy has mapped and mentioned all the norms and guidelines required to set up a Chemotherapy or Oncology center. If you need any further assistance in designing Hospitals, or a refined market and financial feasibility or any other study related to healthcare you can Contact Hospaccx Healthcare Consultancy Business on hospaccx.india@gmail.com or you can visit our website on hospaccxconsulting.com.
INTRODUCTION
Change affects all areas of healthcare organizations and none more so than each aspect of the oncology ward, beginning with the patient’s room. It is there that the issues faced by the major players in healing environments – administrator, caregiver, family member, and, most importantly, the patient – come sharply into focus. Hospitals are building new facilities or renovating old ones in order to adapt to new environmental demands of patient care and security.
The treatment of cancer is complex, often involving a combination of treatment methods to be effective. The following methods may be provided, alone or in combination, as part of an individual’s management plan:
- Surgical intervention
- Chemotherapy
- Radiation Therapy
- Hormone Therapy
Chemotherapy is prescribed for the treatment of diseases, especially cancers, using specific cytotoxic agents or drugs that are destructive to malignant cells and tissues. The Medical Oncology (Chemotherapy) Unit provides for the clinical treatment and management of patients undergoing Chemotherapy treatment for cancer. The function of the Unit may include:
- Chemotherapy Administration
- Administration of blood products and/or other supportive therapies
- Blood collection
- Clinical procedures and examination
- Patient and family education and support
- Clinical trial management
- Coordination of care
Support services that are associated with the chemotherapy service may include:
- Physiotherapy (including lymph edema management)
- Occupational therapy
- Dietetic / Nutrition services
- Clinical Psychology
- Social work services
- Community and outreach cancer services
- Palliative Care
- Complementary therapies (e.g. relaxation, stress management and massage)
- Wig and prosthesis services.
Planning should address the following key issues:
EXTERNAL
- Ease of access to the unit where the majority of people will arrive by car on a daily basis.
- Separation of walking and stretcher/ambulance patient arrivals
- Safe access to the unit’s storerooms for the delivery of bulk items e.g. Bulk fluids which may arrive or be stored on a palette requiring mechanical lifting, moving and storage
- Safe access for the delivery of food, clean linen, pharmacy, consumables, disposable items and the removal of bulk cytotoxic chemotherapy waste and soiled linen etc.
INTERNAL
The internal planning of the Chemotherapy Unit should be planned by considering the units functional areas/zones.
Some of the critical relationships to be considered include:
- Staff station/s require an unobtrusive view of all patient treatment areas. The inclusion of decentralized staff stations may be considered in larger units that have multiple treatment spaces
- Providing a number of treatment spaces and/or individual cubicles in groups or clusters
- Inclusion of working spaces for visiting multidisciplinary team members.
- Location of Reception to provide a clear view of entry and exit/egress points of the Unit
- Easy access from the Waiting area to the patient treatment area for the convenient arrival and departure of patients and families
FUNCTIONAL AREAS
The Chemotherapy Unit may include the following Functional Areas:
- Entry / Reception including:
- Waiting areas with amenities such as beverage making facilities, telephones, vending machines, play area for children and toilets
- Interview room for patient/ family discussions and treatment planning
- Storage for files, stationery, wheelchairs
- Chemotherapy Treatment Areas including:
- Treatment chair or bed bays
- Isolation rooms as required
- Ensuites, Patient Toilets
- Treatment Room
- Cytotoxic room
- Support Areas including:
- Bays for linen, resuscitation trolley, mobile equipment
- Clean and Dirty Utilities
- Cleaner’s and Disposal rooms
- IT/ Communications room
- Staff Station
- Storerooms for equipment, general supplies
- Property bay for patients
Entry /Reception:
The Reception area will provide for administrative tasks, such as booking appointments and record keeping, as well as receiving and directing patients to the appropriate zone for consulting or treatment. The waiting area should accommodate a range of patients and visitors with varied levels of ability and provide clear access to conveniently located public and patient amenities, including toilets and parenting rooms. A child play area can be incorporated into the main waiting area. Facilities for volunteers and transport staff may also be provided in this area.
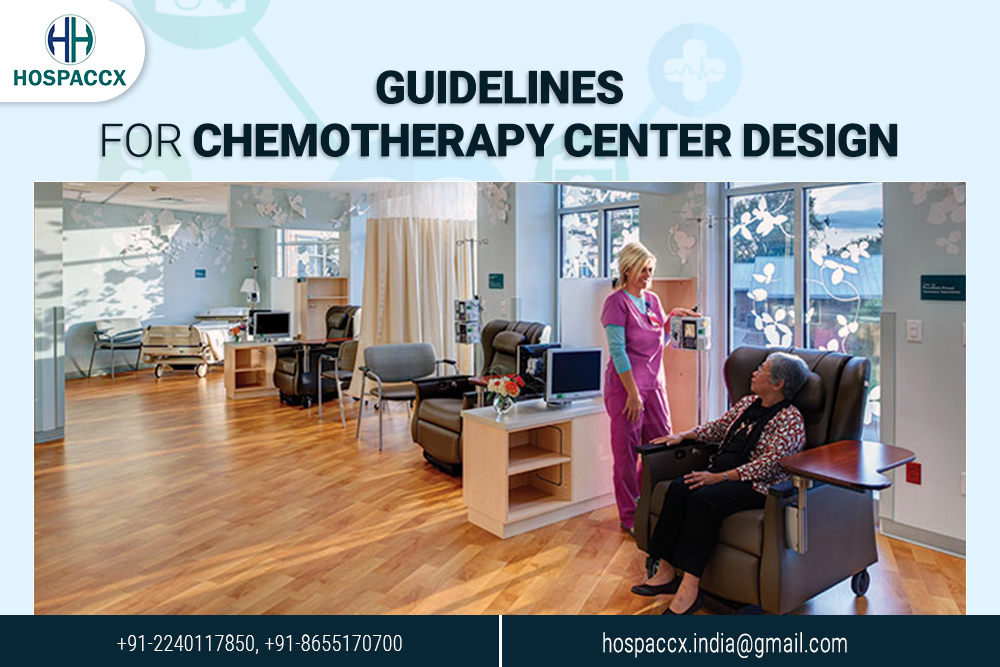
Patient Bed/ Chair Bays:
Patient Treatment Areas should be planned to provide staff members with direct visualization of patients in treatment bays. The preferred design is to locate staff stations in the centre of the treatment spaces to allow a direct line of vision between patients and staff. Beverages and refreshments should be accessible to patients. In large Oncology Units, patient areas may be divided up into clusters of 6 – 10 chairs with small decentralized staff stations. Lounge areas may also be provided to provide patients with choices regarding where they spend their time during treatment. Standard pressure Isolations rooms should be provided for use by patients who are infectious or require reduced contact due to compromised immune systems. Negative pressure isolation rooms may be used dependent on service plan requirements.
Support Areas:
Support areas include clean and dirty utilities, storage, disposal rooms, linen bays, personal protective equipment bays and handwashing facilities. Emergency support, including resuscitation equipment should be located close to centrally located staff stations to ensure rapid access in emergency situations and emergency shower and eye washing facilities should be located close to patient areas for use in case of spills of cytotoxic chemicals. For a Stand-alone facility, support areas also include Back of House areas such as Loading Docks, Waste Compactors and Recyclables, Bulk Storage and Gas Bottle Storage (if medical gases are required).
ENVIRONMENTAL CONSIDERATION
Acoustics:
- Location of the unit away from noisy hospital areas
- Use of sound isolating construction and selection of sound absorbing materials and finishes
- Planning to separate quiet areas from noisy areas
- Review of operational management and patient/client flows; this may include separate areas for patients with special needs
- Provision of television systems with headphones to reduce ambient noise levels
Natural Light/ Lighting:
- Natural light and views should be available from the Unit for the benefit of staff and patients. Every effort should be made to provide a view to all treatment areas either by locating treatment bays/ cubicles/ bedrooms adjacent to a window or by locating chairs and beds to have an external view from each patient space. High quality task lighting is essential to ensure complex medical and pharmacological tasks can be safely achieved. Colour corrected lighting is also essential to ensure patient assessment can be conducted effectively.
Interior Décor:
Interior decor includes furnishings, style, colour, textures and ambience, and is influenced by perception and culture. The décor of the Unit should provide an inviting and comfortable space with a non-institutional atmosphere. Cleaning, infection control, fire safety, patient care requirements and the patients’ perception of a professional environment should always be considered. Suggestions to achieve this balance include the following:
- Use of design features such as colours and artworks to distract the sight from clinical areas
- Inclusion of soft furnishings that act as a design feature such as screening, lounges in waiting areas and window treatments
- Provision of corridors at the required widths for patient access and services deliveries
- Provision of a beverage bay for people to use while waiting
- Provision of background music through a piped system or a centralized unit that can contribute to Unit ambience.
Heating, Ventilation, Air-conditioning (HVAC):
Air conditioning systems should be designed with consideration to provision of appropriate air exchanges and exhaust for cytotoxic chemicals. The temperature of the unit should be maintained within a comfortable range not exceeding 25 degrees Celsius for optimal operating efficiency and patient comfort. General air conditioning outlets should not be placed directly over patients on chairs, beds or trolleys.
Nurse Call, Emergency Call, Duress Alarms:
Nurse Call and Emergency Call facilities shall be provided in all patient areas such as bed/ chair spaces, toilets, bathrooms, consult rooms and treatment rooms for patients and staff to request urgent attention. The individual call buttons shall activate the annunciators and central module situated at or adjacent to the Staff Stations in a discreet manner.
Provision of a Duress Alarm system is required for the safety of staff members who may occasionally face threats imposed by clients/ visitors. Call buttons will be required at all Reception/ Staff Stations, consult rooms and Treatment rooms where a staff may spend time with a client in isolation or alone. The combination of fixed and mobile duress units should be considered as part of the safety review during planning for the unit.
Medical Gases:
Medical gases (oxygen and suction) outlets should be provided to the following for use in patient emergencies:
- Bed spaces
- Chair spaces, may be shared between two chair spaces
- Treatment and Procedure rooms.
Infection Control:
Oncology patients are at increased infection risk due to immunosuppression and frequent exposure to healthcare settings. Flooring, walls, furniture and fittings should be carefully selected to ensure effective infection control measures.
Infectious and immune-suppressed patients may occupy the same treatment space at the different times of the same day. The design of all aspects for the Unit should take into consideration the need to ensure a high level of infection control in all aspects of clinical and non-clinical practice.
Chemotherapy Waste Disposal:
Chemotherapy pharmaceuticals are highly toxic and designated as dangerous waste. All bulk chemotherapy waste is hazardous waste and must be disposed of at a dedicated waste facility. Chemotherapy wastes include:
- Expired drugs and aborted dosages
- All equipment used in preparing and delivering chemotherapy drugs to patients
- Contaminated personal protective equipment (PPE) and other materials.
CONCLUSION
The above mentioned are the minimum standard requirements to design or set up a Chemotherapy center. This study concludes that minimum designing guidelines need to be followed by the architect to design the Chemotherapy center.
For further details contact us at Hospaccx Healthcare business consulting Pvt. Ltd on hospaccx.india@gmail.com or you can visit our website on hospaccxconsulting.com
Related Team Members